Have you ever thought about how antibiotics you take when you’re sick might be affecting more than just your symptoms? Let’s dive into the intriguing world of “The Link Between Antibiotics and Gut Health.”
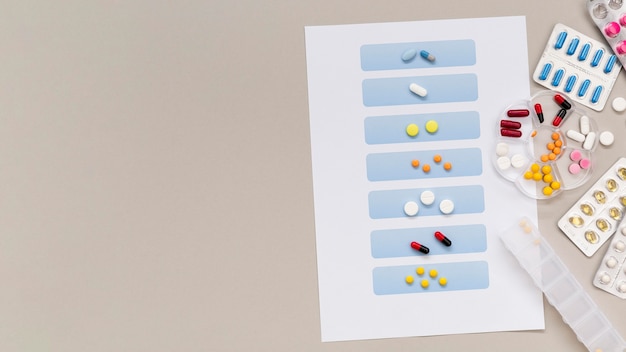
These tiny pills don’t just target the bad bacteria causing your illness; they also impact your gut. Picture it as a microscopic party in your digestive system, and we’re about to explore how it influences your overall health. So, let’s uncover the secrets of your gut and how antibiotics surprisingly play a role in its balance.
Your gut microbiome is a vibrant community of trillions of microorganisms living in your digestive tract, including bacteria, viruses, fungi, and other microbes. This diverse ecosystem helps with digestion and affects your immune system, metabolism, and even mental health. The makeup of the gut microbiome varies among people, influenced by factors like genetics, diet, and the environment.
Antibiotics are designed to fight bacterial infections, but they’re not picky. While they attack harmful bacteria, they can also disrupt the beneficial microbes in your gut. This disturbance can lead to an imbalance known as dysbiosis, where the equilibrium between different bacterial species is thrown off, potentially leading to various health issues.
In the short term, antibiotics can cause immediate changes in the gut microbiome, wiping out both harmful and beneficial bacteria. This makes your gut vulnerable to opportunistic pathogens, leading to digestive problems like diarrhea, bloating, and abdominal discomfort. The severity of these side effects depends on the type of antibiotic and your individual susceptibility.
The long-term effects of antibiotic use on gut health are still being studied. Some research suggests that repeated or prolonged antibiotic use can cause lasting changes in the microbiome, contributing to chronic conditions like irritable bowel syndrome (IBS), inflammatory bowel diseases (IBD), and metabolic disorders.
Beyond their impact on the gut microbiome, antibiotics contribute to the global issue of antibiotic resistance. Overuse and misuse of these drugs lead to the development of resistant bacterial strains, making antibiotics less effective. This growing problem is a significant public health concern, limiting treatment options and increasing the need for stronger antibiotics.
As we become more aware of the link between antibiotics and gut health, interest is growing in strategies to minimize negative effects. Probiotics—live microorganisms that offer health benefits when taken in appropriate amounts—are gaining attention for their potential to restore the gut’s balance. Healthcare providers are also exploring targeted antibiotic therapies to reduce microbiome disruption.
Diet also plays a vital role in shaping the gut microbiome. During and after antibiotic treatment, a diet rich in fiber, prebiotics, and fermented foods can help restore a healthy gut. These dietary components provide essential nutrients for beneficial bacteria to thrive, aiding the recovery of the gut ecosystem.
While significant progress has been made in understanding the connection between antibiotics and gut health, there are still many unknowns. Research is ongoing into how specific antibiotics affect different bacterial strains and how these changes impact overall health. Unlocking these mysteries could lead to more personalized antibiotic treatments that minimize harm to the microbiome.
The impact of antibiotics on children’s gut health is crucial. Pediatric populations, with their developing microbiomes, may be more vulnerable to long-term antibiotic effects. Emerging studies highlight the potential consequences of early antibiotic exposure, emphasizing the need for careful antibiotic use in pediatric healthcare to protect future generations’ health.
The use of antibiotics also has environmental ramifications. Widespread use in agriculture, livestock, and aquaculture spreads antibiotic residues into the environment, contributing to antibiotic-resistant bacteria in natural ecosystems. Understanding these environmental impacts is essential for adopting sustainable practices that balance effective treatment with ecological preservation.
In summary, taking antibiotics can be like inviting a party-crasher to your gut. They help fight bad bacteria but can also disrupt the good ones, causing an imbalance in your gut’s ecosystem. So, next time you’re on antibiotics, think about giving your gut some extra care—perhaps with some probiotics—to keep things balanced. Cheers to a happy and healthy gut!
**How do antibiotics affect gut health?**
Antibiotics influence gut health by upsetting the balance of bacteria in the digestive system. They target harmful bacteria causing infections but also impact beneficial bacteria crucial for a healthy gut. This disturbance can lead to digestive issues like diarrhea or upset stomach as the microbial community in the gut temporarily changes.
**How long does it take your gut to recover from antibiotics?**
The recovery time for the gut after antibiotics varies from person to person. Generally, it takes a few weeks for the gut microbiota to return to its normal state. During this time, consuming probiotics like yogurt or fermented foods can help replenish beneficial bacteria and support overall gut health.
**Can antibiotics inflame the gut?**
Yes, antibiotics can potentially inflame the gut. They can impact the lining of the gastrointestinal tract, leading to inflammation and symptoms like abdominal discomfort or bloating. It’s important to be mindful of these effects and take steps to support gut health during and after antibiotic use.